by Isabella Blakeley (’26)
In the United States alone, it is estimated that 6.7 million people suffer from Alzheimer’s disease. Worldwide, however, that statistic bubbles to nearly 55 million Alzheimer’s sufferers. Alzheimer’s disease is a progressive degenerative disease that causes brain cells and connections to these cells to die, which destroys memory functions and other necessary motor skills. There are three main stages of Alzheimer’s: early stage, middle stage, and late stage. Ultimately, Alzheimer’s is completely fatal for those diagnoses. Currently, the cause of Alzheimer’s disease is not well understood. Doctors have many hypotheses such as long-term alcohol abuse or genetic and lifestyle factors, but do not currently have a concise theory on what causes the disease. In light of this, many neurologists have discovered new ways to help treat the symptoms of Alzheimer’s. One of these treatments is called DBS meaning Deep Brain Stimulation. While DBS is showing promising results, it is one of the more ethically and morally debatable treatments.
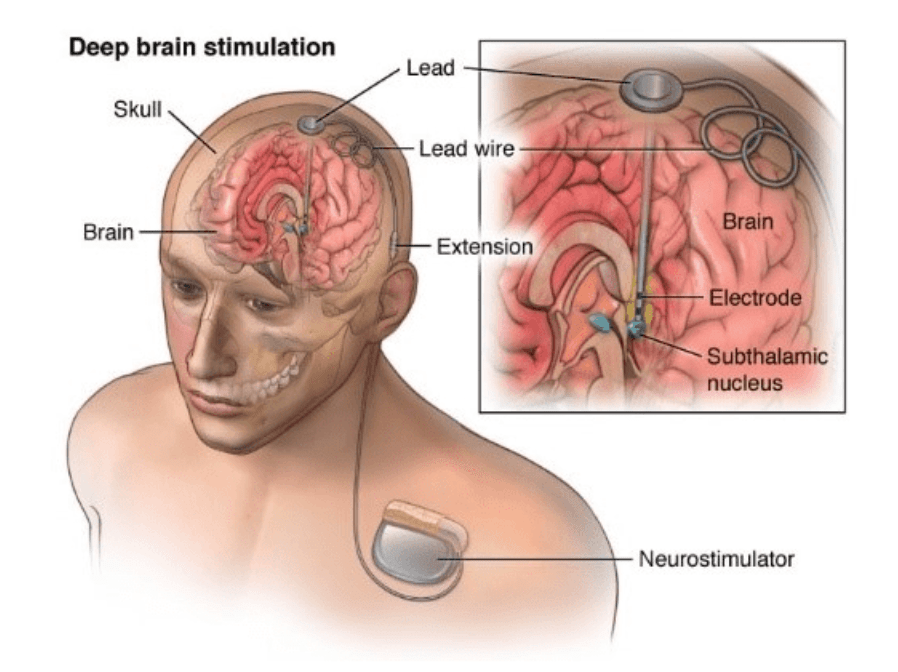
DBS or Deep Brain Stimulation is a procedure where electrodes, electrical conductors, are placed artificially into specific brain regions. The electrodes are connected to an electrical device in the patient’s chest cavity. This creates the electrical pulses that override the abnormal electrical brain impulses that a patient with Parkinson’s disease would have. While it does not cure the patient of the disease, a study in 2018, along with a more recent study in 2022, show that the addition of DBS along with standard dementia care and therapy helps to slow the progression of dementia as well as slows the symptoms. In addition to treating Parkinson’s disease, DBS has also shown promise in patients with tremors as well as OCD. However, DBS is considered controversial and invasive as opposed to other dementia and Alzheimer’s treatments.
According to Johns Hopkins medical journal, DBS can help to reduce tremors, stiffness, and slowness, while also slowing the progression of the disease. In addition, this procedure could reduce the amount of medication that a patient needs. According to Healthline, up to 75% of the patients felt that their symptoms were managed more effectively with the DBS than without. Also, at an earlier stage, it is said to improve the quality of life and also the duration of the patient’s life by a small amount. In addition, the DBS has helped to improve many other conditions such as OCD, dystonia, and other conditions that affect people’s neuro. The effects of DBS can last up to fifteen years after the device is implemented, meaning that patients can live a more comfortable life throughout all the stages of the disease.
Unfortunately, there are many downsides to the DBS device. The surgery is invasive for the patients, and while the surgery itself is not intolerable, the recovery could take eight weeks before other medication starts to work again. The side effects of DBS are to be expected, with the most common being brain lesions, hemorrhage, strokes, and illnesses. It is also common for the electrodes to be rejected by the brain cells and kill cells and connections within the patient’s brain. Many of the surgeries need to be followed up by requisite surgeries to fix the electrical device in the chest wall. As it’s similar to a pacemaker, dizziness, and infection may occur with the device. Not only are there many risks with the devices, but the price of the device can balloon up to 100,00 dollars for patients. And even if money may not be a problem for some, there are still many other ethical concerns with Alzheimer’s patients.
As Alzheimer’s is a cognitive decline illness, and will eventually cause the patient to die, many people are worried about the ethical implications of the device’s implications. Many Alzheimer’s patients are older, with 90% of cases occurring in people 65 or older, and often, the device is put in during the first or second stages of the disease. Unfortunately, many patients do not have the cognitive ability to decline the device if they do not wish to have it implanted. This is because many of the Dementia and Alzheimer’s patients’ family members take care of them. They can make medical decisions for their ill family members and sometimes do not listen to the patient’s actual medical wishes. Unfortunately, many of the patient’s wishes are not supported, and instead, are pushed towards pursuing a longer life duration instead of the comfort and safety that they sought in the first place.
While Deep Brain Stimulation is a new and promising technology, the treatment has many pros and cons. The stimulation allows for an improvement of symptoms and a longer life expectancy. In addition, DBS has proved to help improve the symptoms for up to 75% of Alzheimer’s patients. However, DBS has many side effects such as stroke or brain lesions, and the machines are very costly to be implanted or replaced. DBS also only helps aid the symptoms instead of helping to improve memory or stop disease progression altogether. Family members may also try to override the wishes of the patient just to prolong their life expectancy. There is still a lot of research to be done to understand the causes and symptoms of Alzheimer’s and dementia. It is clear, however, that the invention of DBS is a huge step in the right direction for creating an Alzheimer’s treatment and, eventually, prevention.
